Metabolic Syndrome (MetS) and Insulin – A Major Health Concern (Part 1)
- Kartikay Dhar
- Sep 13, 2025
- 5 min read
This is the first part of a two-part series on Metabolic Syndrome (MetS).
Part 1 will cover what is currently known and accepted about this condition.
Part 2 will discuss possible approaches to reversing it, rather than only managing it with long-term medications such as Metformin—a path that can sometimes feel self-defeating.
Why Metabolic Syndrome Matters

Metabolic Syndrome (MetS) is one of the biggest yet least-discussed health challenges today. It increases the risk of diabetes, heart disease, stroke, and even certain cancers.
The surprising fact is that awareness remains low—yet a large portion of this condition can be managed (and even prevented) through dietary changes, lifestyle improvements, and early interventions. If we do not discuss it openly, how will we find solutions?
This series is an attempt to demystify MetS and highlight workable solutions.
A Brief History
The term Metabolic Syndrome was institutionalized in 2001, when it received the ICD-9 code 277.7. At that time, it was recognized as a first-order threat for developing atherothrombotic complications (blood clots forming on top of artery plaque, obstructing blood flow, and leading to conditions like heart attack or stroke).
Although the concept is only around 40 years old, we still don’t fully understand all its causes.
The Challenge of Defining Numbers
One of the main difficulties in assessing the true prevalence of MetS is that multiple definitions exist.
For example:
A 2011 study in India, applying the NCEP: ATP III criteria, found that 95% of the examined population had at least one abnormal parameter, with an overall prevalence of BMI abnormalities at 79.1% (Jha et al., 2021).
This variability makes comparisons and clear statistics difficult, but the direction is obvious: the numbers are alarmingly high.
Mechanisms of Insulin Resistance and Glucose Intolerance

At the core of MetS is insulin resistance—a condition where the body’s cells no longer respond effectively to insulin.
In normal physiology, insulin acts like a key, unlocking cells so glucose can enter and be used for energy.
In insulin resistance, the cells fail to respond, so the pancreas compensates by releasing more insulin (a state known as hyperinsulinemia).
Over time, this mechanism fails, leading to elevated blood glucose levels—the defining feature of glucose intolerance.
What Is Blood Glucose?
Blood glucose (blood sugar) is the main sugar found in the blood and the body’s primary energy source.
It comes from the food we eat.
The body breaks food down into glucose and releases it into the bloodstream.
Rising blood glucose signals the pancreas to release insulin, which then manages sugar fluctuations.
When this delicate relationship deteriorates, long-term metabolic disorders develop.
The Growing Burden
“The increase in metabolic risk factors—elevated blood pressure, obesity, hyperglycemia, and hyperlipidemia—are contributing to an emerging pandemic of non-communicable diseases (NCDs).” (Shivani Rao et al., 2025)
According to the Global Burden of Disease Study (2019), mortality rates from diabetes and obesity have not improved since 1990.
In India, NCDs caused 61.8% of annual deaths in 2016.
India now has:
100+ million people with diabetes
36% prevalence of hypertension (HTN)
50% prevalence of dyslipidemia
Urban India shows a much higher prevalence than rural areas, especially among economically underprivileged groups.
It is estimated that 30% of the population already falls within the MetS zone. But if we remove the blurred overlap between those “controlled by medication” and “free-fall” groups, that percentage could be much higher.
Risks Associated with MetS
5x greater risk of developing Type 2 Diabetes
2x greater risk of developing cardiovascular disease within 5–10 years
2–4x greater risk of stroke
3–4x greater risk of myocardial infarction (heart attack)
2x greater risk of death compared with those without MetS

The Meaning of "Syndrome"
The word comes from the Greek “Sundromos”—“to run together.”
Metabolic Syndrome is exactly that: multiple metabolic abnormalities running together, including:
Dyslipidemia (abnormal fat metabolism)
Obesity
Glucose intolerance
High blood pressure
Pro-inflammatory and pro-thrombotic changes
Together, these interconnected disturbances significantly raise the risk of coronary heart disease, type 2 diabetes, and premature death.
Insulin Resistance – The Core Problem

At the center of MetS lies insulin resistance.
How it Works Normally
Insulin allows glucose (sugar) to move from the blood into cells for energy.
It signals the liver to store excess glucose as glycogen.
It prevents the liver from overproducing sugar.
What Goes Wrong
In insulin resistance:
The cells stop responding properly to insulin.
The pancreas produces more insulin to compensate (hyperinsulinemia).
Over time, this fails, leading to chronically high blood glucose levels (glucose intolerance).
What Happens in the Body During Insulin Resistance
Insulin’s primary role is to regulate blood sugar by allowing glucose to move from the bloodstream into cells.
After meals, insulin:
Helps glucose enter cells for energy
Signals the liver to store excess glucose as glycogen
Prevents the liver from producing too much sugar
When this balance breaks down, two problems arise:
Blood sugar levels rise without enough insulin to counterbalance them
Or, communication fails, and the pancreas does not release enough insulin
Both scenarios define insulin resistance.
Insulin Resistance Across Tissues

Skeletal Muscle
Skeletal muscle accounts for up to 80% of post-meal glucose uptake.
Muscle insulin resistance is considered the primary defect in Type 2 Diabetes.
Aging reduces glucose regulation ability and causes muscle atrophy, increasing the risk.
Liver
The liver controls carbohydrate levels by:
Suppressing glucose production (gluconeogenesis)
Storing glucose as glycogen after meals
In insulin resistance, the liver fails to suppress glucose production, worsening hyperglycemia.
This is often linked to defective fat metabolism in adipose tissue.
Adipose Tissue
Fat cells are of three types: white (stores energy), brown, and beige (burn energy).
Healthy balance between these is crucial.
Insulin resistance disrupts this balance, contributing to abnormal fat metabolism.
Endothelium (Blood Vessels)
Insulin normally stimulates the production of nitric oxide (NO), which increases blood flow to muscles and enhances glucose uptake.
In insulin resistance, this mechanism is impaired:
Reduced NO production
Increased endothelin-1 (ET-1), which constricts vessels
The result: decreased blood flow, oxidative stress, and inflammation.
Beyond Diabetes – Links to Cancer
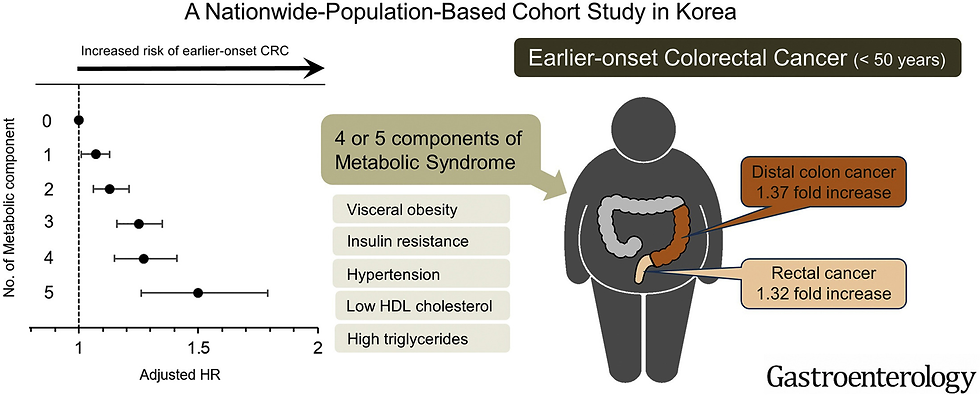
Research suggests that insulin resistance may be a primary driver of cancer-associated metabolic dysfunction.
It increases the risk of cancer recurrence and mortality.
Higher risks are observed for:
Breast cancer
Colorectal cancer
Liver and pancreatic cancers
Endometrial cancer
Lung and prostate cancers
In other words, insulin resistance not only contributes to diabetes and heart disease but also worsens cancer outcomes.
✅ Part 2 will dive deeper into what is currently known about reversing insulin resistance and metabolic syndrome—beyond conventional management with medications.



Comments